Skin Infections
Identify underlying disease as skin infection is ALWAYS secondary
Antibiotics are not indicated for
- Malassezia dermatitis
- Ectoparasites
- Pruritus
- Anal sac impactions
Surface pyoderma (hot spots & intertrigo)
Topical treatment ONLY
- 2–4% chlorhexidine or other antiseptics q1–3d
If not responsive or very severe
- Fusidic acid ± glucocorticoid (cocci)
- Silver sulphadiazine (if rods)
Superficial pyoderma
Topical treatment ONLY is appropriate
Review after 2–3 weeks and continue until underlying cause
controlled
- 2–4% chlorhexidine q1–3d
If non-responsive to topical antibiotic therapy
- Clindamycin
- Trimethoprim/sulphonamide
- Cefalexin
- Amoxicillin/clavulanate
Systemic antibiotics ALWAYS in combination with topical antiseptics
(q1–3d)
Treat for 2 weeks then reassess. If poor response investigate resistance (cytology, culture and susceptibility testing)
Use doses at upper end of range
ALWAYS culture if there is a history of MRSP/MRSA OR prior antibiotic courses OR if rods are seen on cytology
Deep pyoderma
Whilst culture and susceptibility testing pending, ONLY start systemic antibiotic (as for superficial pyoderma) if painful OR risk of septicaemia
- Concurrent topical treatment with 2–4% chlorhexidine q1–3d
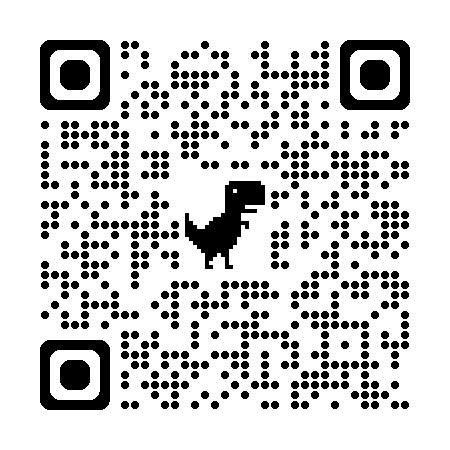
Treat for minimum 3 weeks and reassess q2w (consult QR code)
Anal Sac Inflammation
Topical treatment ONLY
- Manual evacuation, flushing with chlorhexidine ± packing with topical polypharmacy ear product (avoid products containing EMA category B antibiotics)
Anal Sac Abscess
Flush and drain as appropriate
ONLY if signs of cellulitis
- Trimethoprim/sulphonamide
- Amoxicillin/clavulanate